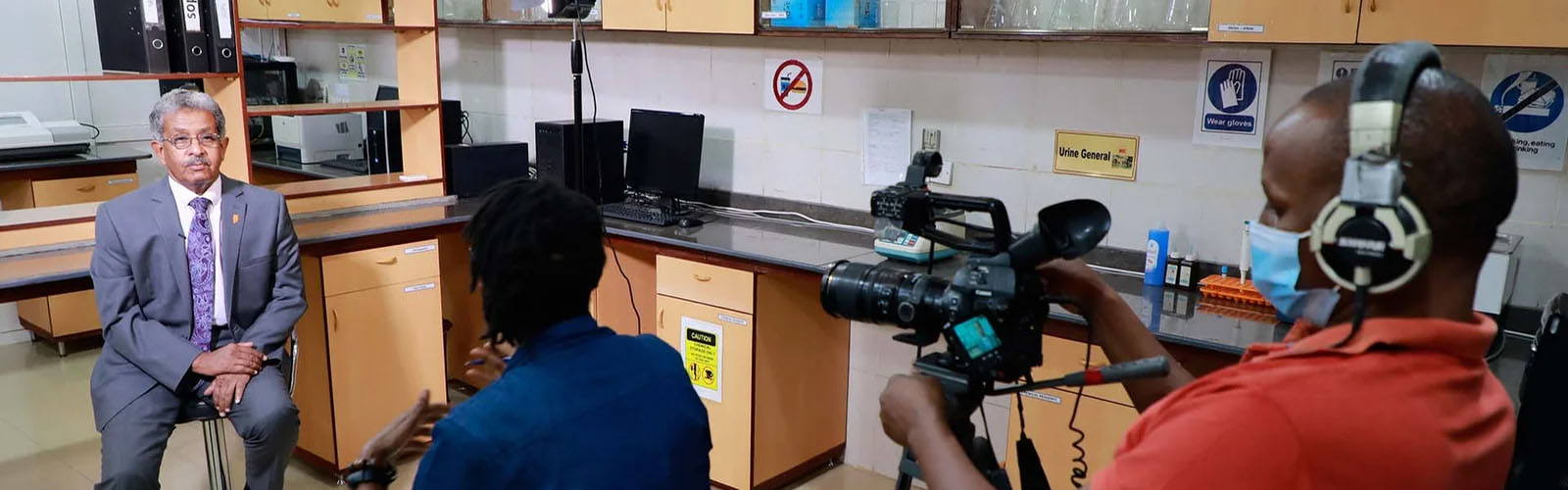
An Inspiring Medical Mission to Ethiopia
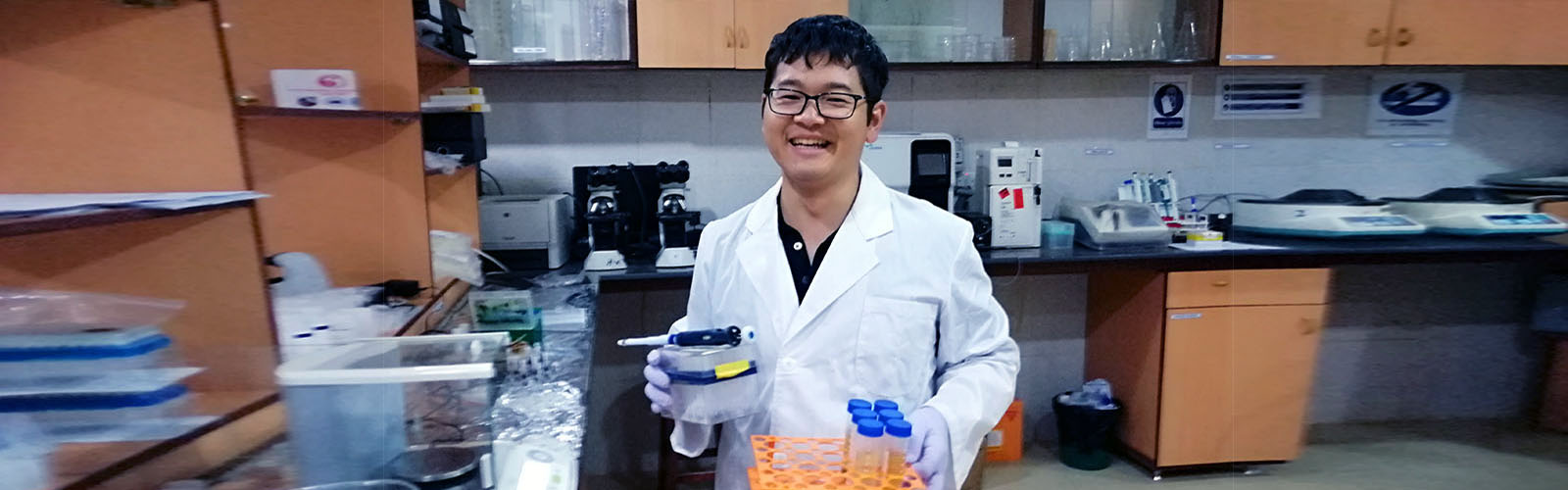
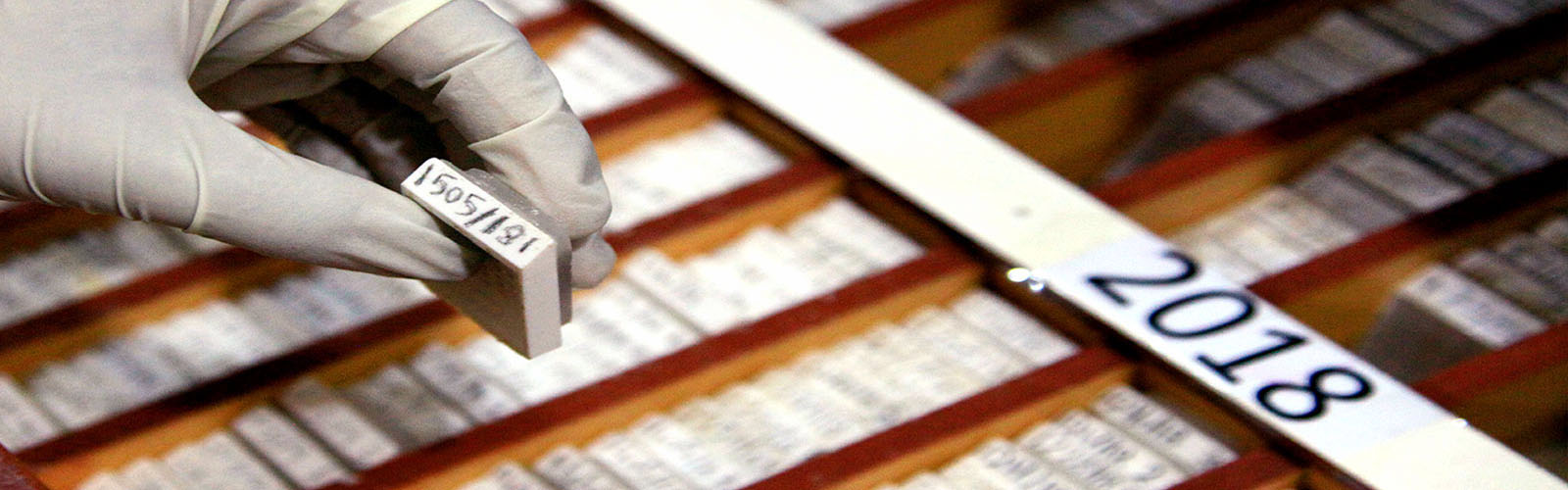
As part of the enduring and impactful collaboration between the Mycetoma Research Center, University of Khartoum, the Drugs for Neglected Diseases Initiative (DNDi), and the Faculty of Medicine at Arba Minch…